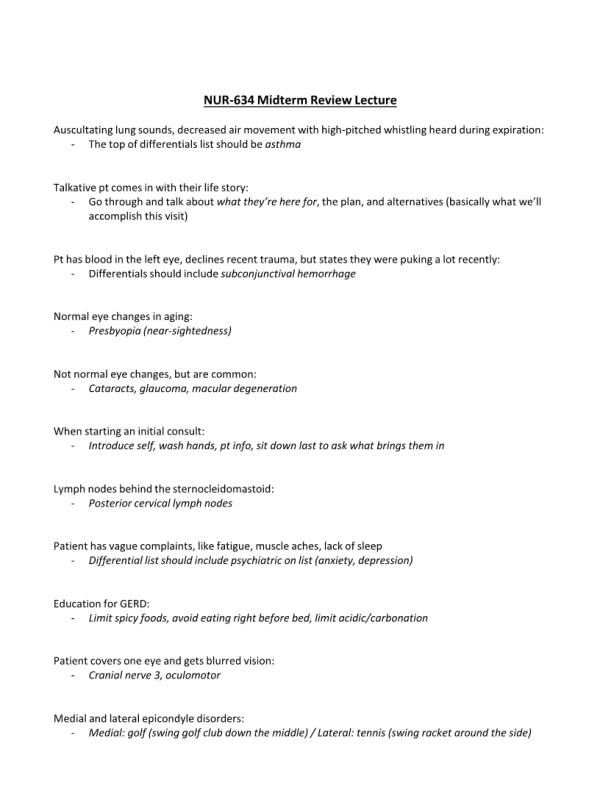
NUR 634 Midterm Reviewn
- $49.00
- Question: Auscultating lung sounds, decreased air movement with high-pitched whistling heard during expiration:
- Question: Talkative pt comes in with their life story:
- Question: Pt has blood in the left eye, declines recent trauma, but states they were puking a lot recently:
- Question: Normal eye changes in aging:
- Question: Not normal eye changes, but are common:
- Question: When starting an initial consult:
- Question: Lymph nodes behind the sternocleidomastoid:
- Question: Patient has vague complaints, like fatigue, muscle aches, lack of sleep
- Question: Education for GERD:
- Question: Patient covers one eye and gets blurred vision:
- Question: Medial and lateral epicondyle disorders:
- Question: Lung sounds:
- Question: Derm; while assessing skin a large lump is noticed, I&D is performed, and a white cheesy substance comes out:
- Question: The patient’s cup-to-disk ratio is 1:2 (not 1:3):
- Question: The patient exhibits chest pain with one single descriptive motion:
- Question: A patient has lost all vision in one eye:
- Question: Tenderness and injury between wrist and thumb:
- Question: PMI landmarks:
- Question: Pt complains of jaw pain- assess for laterality, ability to chew, any clicking:
- Question: Obtaining social history:
- Question: A parent worries their young child is experiencing hair loss, ask/assess for:
- Question: On physical exam, patient has ‘spiderweb veins’ up their neck (spider hemangiomas):
- Question: Meningitis s/s:
- Question: Soft palate cranial nerve:
- Question: Small, moveable mass:
- Question: Sty:
- Question: A patient has a history of lupus and new-onset rash on legs that are reddened:
- Question: Questions to ask a woman / assess during complaints of incontinence to assess underlying cause:
- Question: Patient complains of should pain, but during provider passive ROM, no pain is exhibited. When patient performs active ROM he feels it:
- Question: A daycare worker becomes jaundiced:
- Question: Silvery, scaly skin condition:
- Question: During abdominal exam, a pulsatile mass is felt:
- Question: Review of systems:
- Question: Dermatology ABCDE assessment:
- Question: Patient complains of a skin finding that began as one large patch, became larger and itchy, and now resembles a Christmas tree:
- Question: During eye exam with pen light, the pupil contracts:
- Question: Friction rub auscultated during heart sounds:
- Question: Unintentional weight loss and fatigue:
- Question: Patient repeats same thing over and over:
- Question: A midline tender, dull mass is palpated during abdominal exam:
- Question: A child presents and begins staring off:
- Question: A patient complains of pain when starting and stopping walking:
- Question: RUQ soft, tender with inspiration, Murphey’s sign positive:
- Question: Ulcerative lesions on feet:
- Question: Patient has a steady hand until nearing grasp of an object:
- Question: At the start of diastole:
- Question: Hallucination vs Delusion:
- Question: Full-thickness injury, damage to subcutaneous tissue, muscle is not affected:
- Question: A patient has lost all interest in activities:
- Question: Patient has thickening of conjunctiva over eyeball:
- Question: Patient experiences dizziness (spinning):
- Question: The one-hour, full head-to-toe assessment should be performed on:
- Question: Abdominal percussion, resonance heard:
- Question: Swimmer’s ear (otitis externa) symptoms:
- Question: CAD risk factors:
- Question: Ecchymosis on forearm for several months without trauma:
- Question: Tinnel sign:
- Question: Someone is over-dramatized and yells out excessively for even the littlest things:
- Question: Left pulses greater than right pulses:
- Question: Know OPQRST (damn script)
- Question: Avoid bringing a computer into patient’s room:
- Question: Pulses are strong to thready, strong to thready, over and over:
- Question: Confirm appendicitis with: