NUR 634 Topic 4 Shadow Health Assignment; Focused Exam; Chest Pain
- $25.00
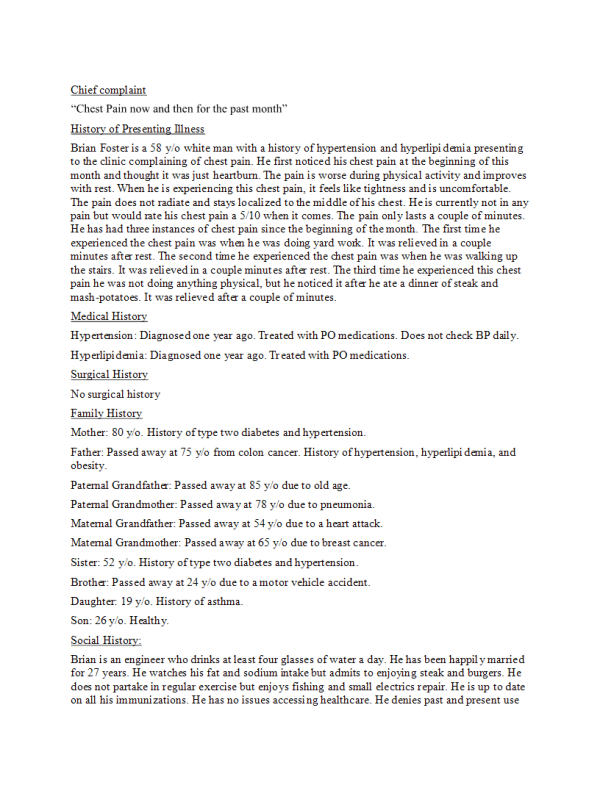
Chief complaint
“Chest Pain now and then for the past month” History of Presenting Illness
Brian Foster is a 58 y/o white man with a history of hypertension and hyperlipidemia presenting to the clinic complaining of chest pain. He first noticed his chest pain at the beginning of this month and thought it was just heartburn. The pain is worse during physical activity and improves with rest. When he is experiencing this chest pain, it feels like tightness and is uncomfortable.
The pain does not radiate and stays localized to the middle of his chest. He is currently not in any pain but would rate his chest pain a 5/10 when it comes. The pain only lasts a couple of minutes. He has had three instances of chest pain since the beginning of the month. The first time he experienced the chest pain was when he was doing yard work. It was relieved in a couple minutes after rest. The second time he experienced the chest pain was when he was walking up the stairs. It was relieved in a couple minutes after rest. The third time he experienced this chest pain he was not doing anything physical, but he noticed it after he ate a dinner of steak and
mash-potatoes. It was relieved after a couple of minutes. Medical History
Hypertension: Diagnosed one year ago. Treated with PO medications. Does not check BP daily. Hyperlipidemia: Diagnosed one year ago. Treated with PO medications.
Surgical History No surgical history Family History
Mother: 80 y/o. History of type two diabetes and hypertension.
Father: Passed away at 75 y/o from colon cancer. History of hypertension, hyperlipidemia, and obesity.
Paternal Grandfather: Passed away at 85 y/o due to old age. Paternal Grandmother: Passed away at 78 y/o due to pneumonia. Maternal Grandfather: Passed away at 54 y/o due to a heart attack. Maternal Grandmother: Passed away at 65 y/o due to breast cancer. Sister: 52 y/o. History of type two diabetes and hypertension.
Brother: Passed away at 24 y/o due to a motor vehicle accident. Daughter: 19 y/o. History of asthma.
Son: 26 y/o. Healthy. Social History:
Brian is an engineer who drinks at least four glasses of water a day. He has been happily married for 27 years. He watches his fat and sodium intake but admits to enjoying steak and burgers. He does not partake in regular exercise but enjoys fishing and small electrics repair. He is up to date on all his immunizations. He has no issues accessing healthcare. He denies past and present use
of tobacco, marijuana, cocaine, heroin, or other illicit drugs. He reports drinking 2-3 beers on the weekend. He drinks 1-2 cups of coffee a day........... Continue